“Aquatic therapy has made me more independent.” This is a quote from a former patient who had approximately twelve weeks of aquatic therapy for low back pain. She had a history of lumbar spine surgery in 2012 but continued to have significant pain and decreased activity tolerance, which eventually put her in a wheelchair. She had tried land physical therapy at other facilities; however, many of her exercises were done in her wheelchair and did not allow her to reach her personal goals. She was eventually referred to aquatic therapy, which she reported was her “last hope.” At the end of the twelve weeks, this patient no longer had radiating pain, which allowed her to reduce the amount of pain medication she was taking. This reduction of pain allowed her to participate in both functional and recreational activities, such as walking with a walker and standing long enough to cook a meal with greater ease and improved balance.


Back patients hold the side of the pool until they develop enough core strength and balance to perform deep water intervals on a tether.
The water was a perfect environment for this patient and for many others with low back pain. Patients with low back pain often start their course of rehab in the water, as there is less impact on the body. The buoyancy of the water helps patients move their limbs more easily through the water, whereas on land they are working against gravity. The buoyancy of the water also decreases weight-bearing, which in turn reduces stress through the joints and intervertebral discs. There is a 50% reduction in weight-bearing in waist-deep water, 75% in chest-deep water, and 100% in the deep end of the pool.
Common diagnoses we may encounter include stenosis, sciatica, degenerative disc disease, and lumbar strain. These diagnoses will help determine a plan of care and can give clues as to which exercises may be painful for these patients. For example, a patient with a diagnosis of stenosis may have increased pain with lumbar extension. Or those with neural tension may have increased pain with forward leg swings or quad extensions at 90 degrees of hip flexion. Post-surgical patients are often referred for pool therapy as well. Common surgical procedures include artificial disk replacement, discectomy, laminectomy and fusion. Be sure all incision sites are fully healed before these patients enter the pool. Also, be mindful of any specific instructions on the prescription.
A typical session for a patient with low back pain will include both deep water and shallow water exercises. For deep water exercises, our patients start with a series of Deep Water Intervals (DWIs), including Bicycle, Powerwalk, and Flies, while holding onto a bar along the side of the pool. Those without bars can hold the coping on the side of the pool. Holding onto the bar or coping allows the patient to maintain trunk stability while focusing on learning correct form, as well as allowing the rehab specialist to assess the patient’s tolerance to the exercises. Once a patient demonstrates good form and control while holding onto the bar, they are ready to transition to the tether. Performing DWIs on the tether incorporates use of the upper extremities and calls for increased core activation to maintain proper form. After DWIs, we stretch. Hamstring stretching may be done in deep water or shallow water and is important for patients with low back pain.
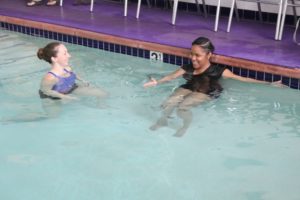
Shallow water exercises typically include both lower extremity and abdominal strengthening exercises. For the lower extremity exercises, patients start by holding onto the bar to improve trunk stability. Make sure that the patient is isolating the proper muscles and keeping the core engaged, as to prevent trunk sway and compensations. A common mistake is activating lumbar spine extensors instead of glutes and hamstrings during Leg Swings. Also keep the depth of the water in mind – if a patient has poor tolerance to weight-bearing, move them to deeper water. If they are still having significant pain, a flotation belt may be worn to off-load the lumbar spine even further.
Once the patient displays proper form and muscle activation without resistance, resistance fins may be used to improve strengthening. Another way to progress lower extremity exercises is to perform them freestanding. This forces the patient to further engage his or her core muscles to maintain upright position, as they no longer can rely on the bar. This also improves single leg balance and glute strengthening on the stance leg.
We also utilize a series of upper extremity exercises that, while incorporating arm movement, forces the patient to engage his or her core muscles. The patient typically starts these exercises braced against a wall, which provides back support when a patient’s abdominal muscles are not yet strong enough. With these exercises, focus on keeping the patient’s back flat against the wall, which is often improved by cuing the patient to rotate his or her pelvis posteriorly. When the back is flat against the pool wall, the proper position has been attained. With time, these exercises can be progressed by increasing the resistance or narrowing the base-of-support.
These exercises can be further progressed by performing them in a freestanding lunge or squat. This forces the patient to engage his or her core muscles since the pool wall is no longer there to support the back. With these exercises, focus on ensuring trunk stability and neutral spine while isolating upper extremity movement. Again, these exercises can be progressed by increasing the amount of resistance used.

Back patients are braced against the side of the pool without resistance as they begin, then add resistance as they progress and finally step away from the wall.
Lower extremity distraction may also be a good way to reduce pain in a patient with radicular symptoms (pain that radiates down the leg). Having weight around the patient’s ankles will provide a traction force to the spine, elongating the muscles of the back and increasing joint space to decrease pressure on the spinal nerves. Contraindications include fractures, acute strains, lumbar instability, post-surgical status, pregnancy, and others. We typically use this method if the patient is unable to tolerate exercise because of severe pain, or if radicular symptoms do not improve after several weeks of aquatic exercise. See below for details on how to set up patients for distraction.

Distraction Technique
- Belt goes on FIRST for safety
- Use 2 belts if heavy weights
- Put on ankle weights in shallow water
- Noodle back to front first; front to back next; use extra noodles rather than extra belts
- If knee sore, move backward, not forward to the deep water
- Add more weight if patient does well
The pool is a great place to initiate the rehabilitation process for a wide variety of diagnoses involving low back pain. Keep in mind the patient’s diagnosis, post-surgical precautions, and current fitness level when creating the appropriate plan of care. The amazing properties of water will allow these patients to strengthen in an environment which may be more tolerable than land, resulting in a speedier recovery.
Katey Eisenstein, DPT, is originally from Pennsylvania and earned her Bachelor of Arts in Psychology at the University of Delaware. She received her Doctor of Physical Therapy at Florida Gulf Cost University where she had considerable experience in outpatient orthopedics as well as acute care and skilled nursing. She performs both pool and land physical therapy as the Clinical Director at CompletePT in Los Angeles.
Lynda Huey, MS, earned a bachelors and masters degree from San Jose State University where she also starred on the track and field team. Her own athletic injuries led her into the water where she learned to cross train and speed the healing of injuries. She has written six books on aquatic exercise and rehabilitation, books that are considered the foundation of aquatic therapy world-wide. Lynda is President of CompletePT Pool & Land Physical Therapy in Los Angeles.

