By Lynda Huey
At 5 AM on Thursday morning, March 16, 2017, spine surgeon Alex Rasouli, M.D. performed the first outpatient surgery to replace a lumbar disc with an artificial disc at levels L4/L5. Although Dr. Rasouli humbly called it “the first in this area,” a search of the internet and phone calls to leading spine centers in Los Angeles and around the country did not turn up a single mention of the surgery being performed on an outpatient basis. This could be the first such surgery or at least one of the very first performed anywhere.
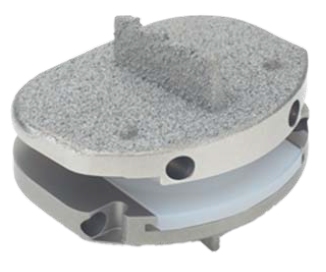
Why is that such a big deal? Actually, it’s two big deals. The first revolutionary change was switching from lumbar fusions to disc replacements. Until recently, the traditional way of treating people who had unmanageable, intractable back pain due to the failure of a disc between L4 and L5 was fusion. Spine surgeons would remove the disk and put in a spacer of bone or plastic, attaching several vertebrae together with screws and rods. That procedure stopped the movement and in many cases also stopped the pain. But sometimes the fusion didn’t heal solidly, and since it was an unnatural thing to fuse a level that was designed to move, issues often arose with the disc above or below the fusion, because those levels now had to compensate for the lost movement. So disc replacements were introduced about ten years ago. They met a lot of controversy because the first few disc replacement devices were failures. The device would come out, or the movement would not be restored, or even worse, some patients had more pain after the surgery than before. Newer-generation devices from multiple companies came out but had trouble getting FDA approval. When the approval finally came, there was trouble getting insurers to pay for it. Medicare, Blue Cross, Aetna and others weren’t paying for the artificial disc replacement surgery, because they still had the bad taste in their mouth from the previous generation of disc replacement devices. Now, as more and more surgeons are doing disc replacements, insurers are becoming more and more willing to accept this new technology, and therefore pay for it. They’ve begun to conclude along with the surgeons that the advantage of disc replacement is that you’re not taking away motion, you’re restoring motion. It’s more natural and has a faster recovery than fusions.

The Prodisc-L is designed to restore normal range of motion in the spine, which can potentially decelerate disc degeneration at adjacent segments of the vertebrae.
The second even bigger big deal is that Dr. Rasouli did this L4/L5 disc replacement in an outpatient setting. He says, “I want people to know that the next five to ten years of spine surgery will be like this: you show up, have your spine surgery, and go home the same day. That was unheard of five years ago, but it’s what we’re doing now. Small surgeries will replace big surgeries, outpatient surgeries are going to replace inpatient surgeries, short recoveries are going to replace long recoveries, and artificial disc replacements are going to replace fusions. That’s the paradigm of the spine for the next five or ten years. Our job is to be the vanguard of this spine movement. We like to avoid surgery as long as possible, but for those few patients on whom we choose to do surgery, we’d rather do smaller surgeries, outpatient surgeries, and disc replacements.
The next five to ten years of spine surgery will be like this: you show up, have your spine surgery, and go home the same day. — Alex Rasouli, M.D, Spine Surgeon
“There’s inertia in the delivery of health care. It takes a while to get things moving. If we can tell the insurance companies that we can do a procedure in an outpatient setting, which costs a lot less than doing it in a hospital, they’re more willing to go along. The patient is much better, because they don’t spend time in the hospital; they go home. They’re not getting fused. They don’t have to wait three to six months for fusion to occur. They’re doing physical therapy within two to six weeks, and they’re getting back to their lives much more quickly.”
Moving from the hospital to an outpatient surgical center was not a step taken lightly by Dr. Rasouli. He said, “I’ve been studying the technique that we’ve been doing in the inpatient setting (in the hospital) for the last five or six years and documenting how much blood loss we had, how long the surgery took, and other details. The L4/L5 surgery used to take two or three hours in the hospital. But once we got the surgery under 30 minutes and less than 5 ccs of blood loss consistently, we decided to do it outpatient. It just takes practice, skill set, and a new mentality that these surgeries can be done in an outpatient setting. There are still cases that are totally and exclusively appropriate for the hospital setting. But these smaller, one-level spine surgeries of the neck or the back are getting to the point where it’s a waste of society’s dollars to do them in the hospital.
Why is the L4/L5 disc so hard to operate on? At L4/L5 level, the blood vessels are running down the center of the body and somebody has to physically move them to the side for the operation on the disc. It takes a team of two equally-skilled surgeons, a vascular surgeon and the spine surgeon, to take part in this advanced surgery.
Dr. Rasouli says, “The incision for the outpatient surgery is about two inches long. For the vascular surgeon to give the spine surgeon safe access to the vertebrae takes about fifteen minutes. Then the actual removal of the damaged disc and replacement takes another fifteen to twenty minutes. The incision heals in a week to ten days. The tissues under that incision have faced minimal trauma at the hand of the surgeon. We don’t go through them or cut them. We exploit the natural anatomical planes of the body to go where we need to go. The tissues separate easily when we’re in a plane. When we’re finished, they fall back into their natural arrangement of layers. It’s not a matter of the tissues between the skin and the spine having to heal.”
This first patient to undergo outpatient L4/L5 surgery walked out of the surgery center that same day. The day after the surgery, he had a little more pain than the day of surgery because the anesthetic was wearing off. His pain was at the incision in the front of the abdomen and at the back where his anatomy had been restored. A week later, most of what he had left was soreness in the back. Two weeks later, there was less soreness in the back.
Without physical therapy the surgery fails.
–Alex Rasouli, M.D., spine surgeon
 Dr. Rasouli continues the update, saying, “About a month to six weeks later, most of the symptoms he’s having are incisional pain in the front, but overall he’s doing very well, walking, sitting, driving, going to work. I asked him not to do any heaving lifting, nothing over fifteen pounds until he finishes physical therapy, which starts six weeks after surgery and continues twice a week for six weeks. Without physical therapy the surgery fails. This is not a fusion; this is a motion restoration procedure and unless the body is trained on how to use that motion, it won’t work. Some patients who have had a fusion will say, ‘I don’t need physical therapy.’ And they might be just fine. But the patients who have disc replacement are different. If they don’t do physical therapy, we’ve just wasted everybody’s time.
Dr. Rasouli continues the update, saying, “About a month to six weeks later, most of the symptoms he’s having are incisional pain in the front, but overall he’s doing very well, walking, sitting, driving, going to work. I asked him not to do any heaving lifting, nothing over fifteen pounds until he finishes physical therapy, which starts six weeks after surgery and continues twice a week for six weeks. Without physical therapy the surgery fails. This is not a fusion; this is a motion restoration procedure and unless the body is trained on how to use that motion, it won’t work. Some patients who have had a fusion will say, ‘I don’t need physical therapy.’ And they might be just fine. But the patients who have disc replacement are different. If they don’t do physical therapy, we’ve just wasted everybody’s time.
“There are a number of reasons why I made such a big push for outpatient surgery. The main reason is because in this environment where it’s so results oriented, the efficiency and value of the care is what everyone looks at – the government, Medicare, the insurers, and the patients. So we need to look at how much good we can do for all of them with the minimum amount of resources. The outpatient setting is perfect because it uses a fraction of the dollars that would be spent if we did the same procedure at a full-fledged hospital.”
Dr. Alex Rasouli has raised the bar high for his colleagues. His steady precision and methodical increase of skill until he was confident enough to do an L4/L5 disc replacement in the outpatient setting will create waves in the orthopedic and neurosurgery world. Let’s watch everyone try to reach the height of the bar.
Water Rehab Specialist, Lynda Huey, MS, earned a bachelors and masters degree from San Jose State University where she also starred on the track and field team. Her own athletic injuries led her into the water where she learned to cross train and speed the healing of injuries. She has written six books on aquatic exercise and rehabilitation, books that are considered the foundation of aquatic therapy world-wide. Her Aquatic Rehab Online Course is being studied by students in 15 countries. Lynda is President of CompletePT Pool & Land Physical Therapy in Los Angeles.
